Vaccines save lives.
Vaccines helped eradicate deadly diseases like smallpox.
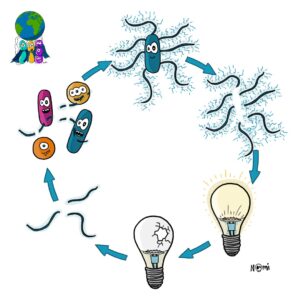
And for over a century, researchers developed vaccines according to Pasteur’s principle. They isolated the microorganism and inactivated it. Then they injected the now harmless microorganism into people.
Now these people were vaccinated.
Their immune systems would detect this foreign microorganism and develop antibodies against it. The next time this person gets infected with the real microorganism, the antibodies would be ready to fight the intruder.
New challenges for researchers
But unfortunately, developing vaccines is not always that easy.
Especially, when researchers have trouble growing an organism in the lab. As it is the case with the hepatitis C virus. And then there are nasty pathogens like Neisseria meningitidis. These know too well how to hide from the immune system and cause deadly meningitis. Or to fight a clever virus like HIV, we need help from extra skilled parts of our immune system. Let alone a virus as SARS-CoV-2 that emerged from nowhere and for which we need a vaccine real quick.
To develop vaccines against these microorganisms, researchers needed a new strategy. They try to find new vaccines that activate the immune system and trigger it to produce antibodies. These antibodies have to detect a specific piece of foreign microorganism. Often, this is a protein from the surface of the virus or the bacterium: the so-called antigen.
But not every antigen is a good antigen that activates the immune system.
Hence, researchers need to produce and test different antigens. And for this, they rely on fancy technologies and super-efficient helpers: bacteria. Here, we will look at how researchers use bacteria in the hunt for vaccines.
Bacterial pets in the lab
For some researchers, the bacterium Escherichia coli is a dear lab pet. They know exactly how to grow, change, regulate, mutate, shock and kill this bacterium. And they appreciate that their favourite lab bacterium can carry big chunks of DNA and produce almost any protein.
So, to produce and test antigens, researchers need to make DNA with a gene for an antigen.
Bacterial machines to produce DNA
To produce any piece of DNA, researchers use a special DNA production machine from the bacterium Thermus aquaticus. This bacterium lives in hot regions, so its enzymes only work at hot temperatures.
Hence, researchers can control this DNA production machine by regulating the temperature. And like this, they can produce any gene they need.
Bacterial machines to cut and paste DNA
The problem is that the gene alone is not stable. This is why researchers need to put this gene (in blue in the picture below) into a plasmid. Plasmids are stable DNA circles (in yellow), that bacteria recognise and produce.
To link these two pieces of DNA together, researchers use special scissors. These scissors cut the gene and the plasmid so that they now work like puzzle pieces. They can only fit together.
These scissors also come from bacteria and, interestingly, every bacterium has its own type of scissors. This means researchers can produce many different puzzle pieces that always work in pairs.
Next, the plasmid and the gene need to be glued together. And for this, researchers use a glue stick from a virus. And yes, it works like the plaster in the picture.
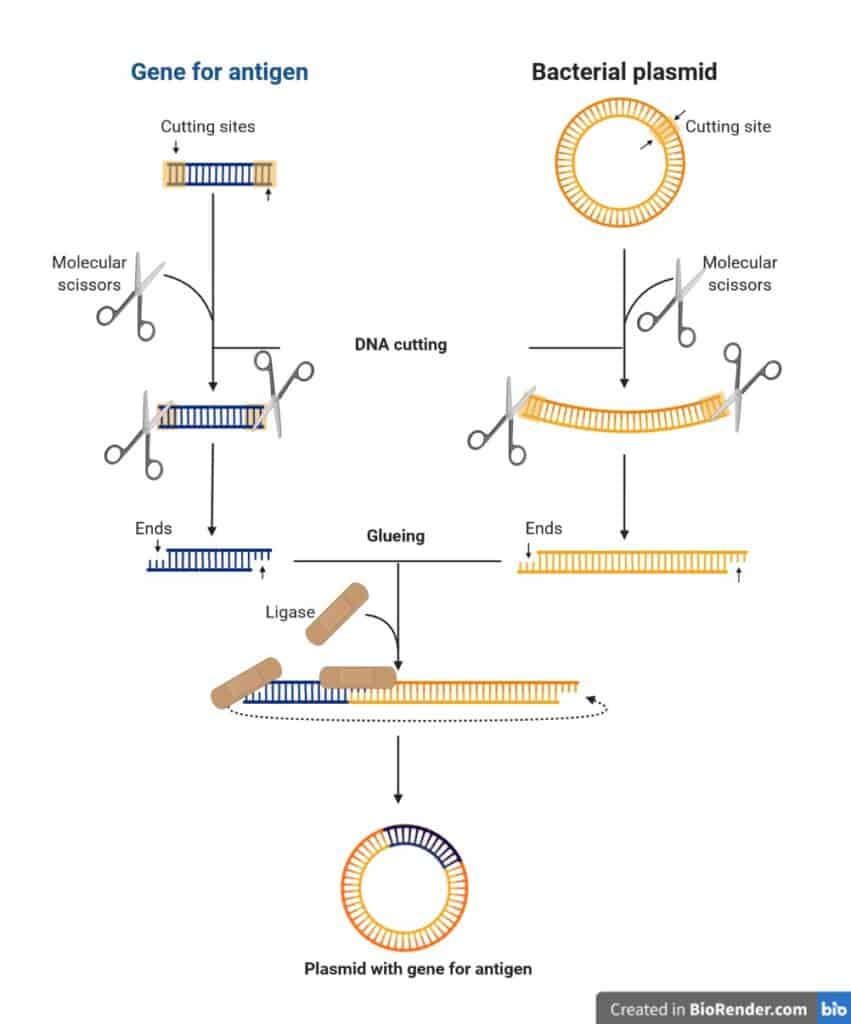
Finally, we have a big chunk of DNA with a gene for an antigen.
Now, researchers need to produce this antigen.
Guess what, they use bacteria for that too!
Bacteria are protein production machines
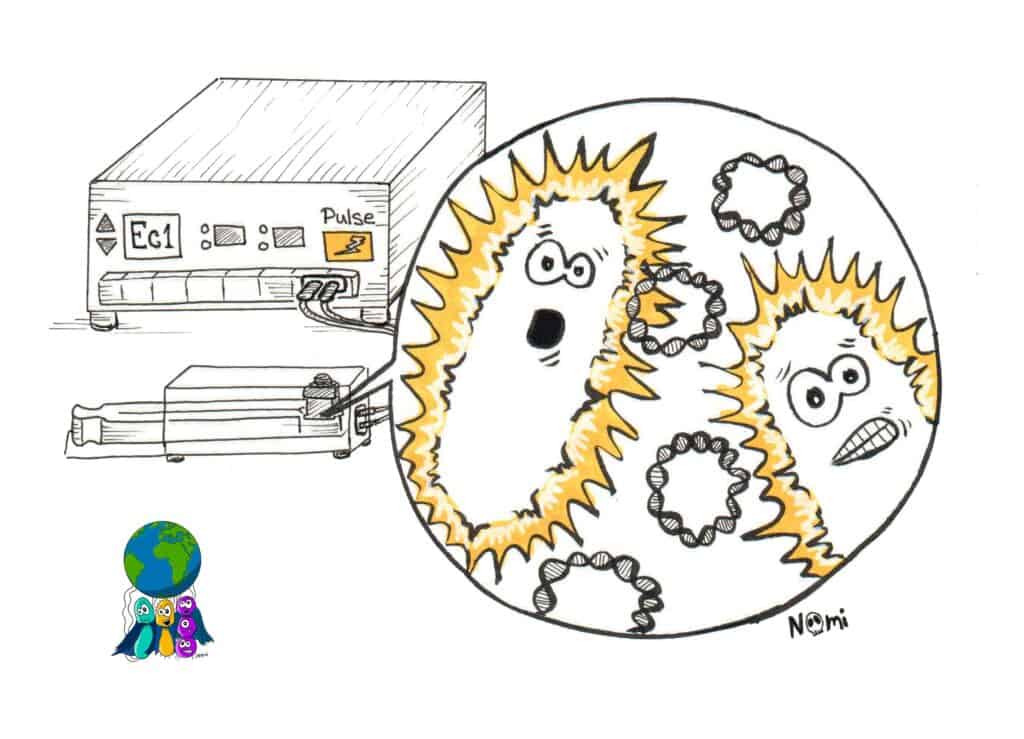
First, the plasmid with the gene for the antigen needs to go inside the bacterial cell. For that, researchers electrocute the bacteria together with the plasmid. Yes, electrocute them! Poor bacteria!
But this brings the plasmids into the bacteria.
Next, researchers grow these bacteria with the plasmid. The bacteria now produce a lot of that plasmid and a lot of that antigen (blue).
Next, researchers need to kill the bacteria and clean the antigens from them.
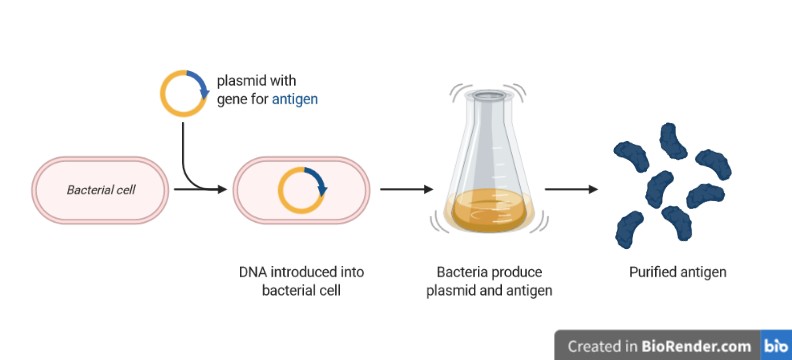
With all the antigens produced now, the fun experiments can get started.
Finding the best antigen for a vaccine
Generally, researchers produce many different antigens to find the best one as a vaccine. The best antigen is the one that binds to an antibody the tightest.
To test all the antigens, researchers do an experiment that is funnily called ELISA. And they can do this ELISA experiment only thanks to bacteria.
Some bacteria from the Streptomyces family produce the protein streptavidin. This protein binds very, very tightly to the vitamin biotin. Obviously, researchers make use of these two proteins in the lab.
In the simplest version of an ELISA experiment, researchers glue antigens to a surface (yellow, blue and green). Then, they add liquids with different antibodies (grey) to these antigens to test which one binds most tightly.
These antibodies are linked to a biotin molecule (grey circle). Next, the researchers add streptavidin (green) that is linked to an enzyme. Now, only if the antibody bound the antigen, the streptavidin can bind the biotin. And if that happens, the enzyme can change the colour of the liquid.
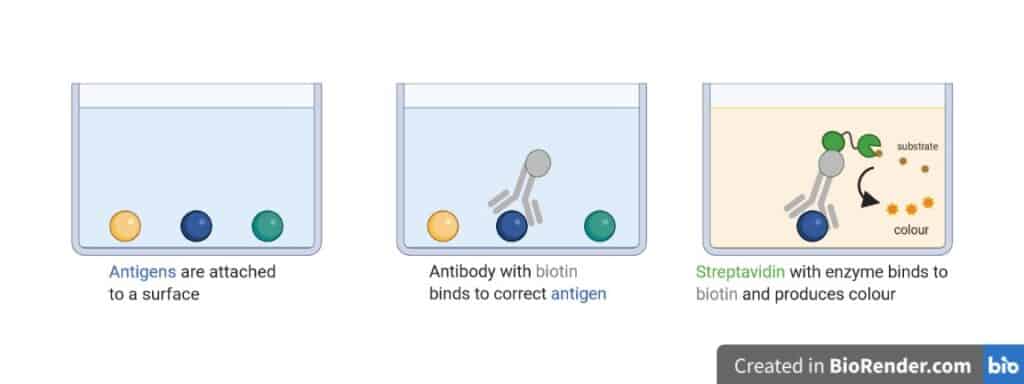
Like this, researchers can test many different antigens and “see” for which the colour changes. These are the ones that bound to an antibody.
Researchers need to repeat all these steps many times; each time changing the antigen a bit to make it more efficient.
But eventually, this antigen becomes a vaccine.
And just as bacteria produced the antigen in the lab, they might have to do that in large amounts to produce the masses of vaccines needed.
About vaccines produced by bacteria
Bacteria can produce different proteins and therefore different vaccines.
For example, the vaccine against the hepatitis E virus is completely made by bacteria. Bacteria produce the envelope proteins of the virus. These then assemble and build the virus structure. This vaccine now has the same structure as the virus, but it is inactive and harmless since no viral DNA is inside the envelope.
Some vaccines also have components from different organisms.
Our immune system can very well detect the sugars on the surface of bacteria. Hence, researchers attach some of these sugars to vaccines. Like this, they attract the big players of the immune system to the vaccine. This activates the immune system so that it develops antibodies against the vaccine.
Researchers also linked bacterial proteins to vaccines. Here, researchers found that bacterial toxins or proteins from the bacterial surface attract and activate the immune system. But not to worry, researchers worked out how to inactivate the toxin so that the vaccine is not harmful.
Not all vaccines are produced by bacteria
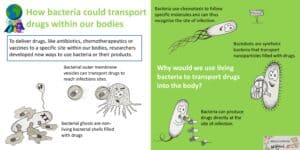
Lastly, researchers developed new strategies to produce vaccines without bacteria. And they even use this strategy for some vaccine candidates against SARS-CoV-2 that causes the COVID-19 disease.
These vaccines only contain a piece of RNA enveloped in a lipid membrane. And, yes, this concept looks a lot like bacterial outer membrane vesicles that transport DNA or drugs.
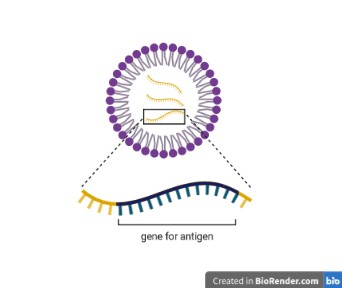
In this case, our body produces the protein – the antigen – from the RNA. This again activates the immune system and triggers it to make antibodies against the antigen.
So while the delivery mode of the vaccine is pretty different, the way to activate the immune system is still the same.
Bacteria are important in the hunt for vaccines
Some microorganisms are real burdens to the world population. Hence, researchers had to come up with new strategies to tackle them. There is no vaccine against the nasty SARS-CoV-2 yet, and maybe the final vaccine will be produced completely independent of bacteria. But still, bacteria are massively helping researchers in the lab.
They are amazing little machines to produce proteins or transport DNA or drugs. And they evolved helpful enzymes that every lab researcher uses daily. No biology-related research would work without the amazing mechanisms of bacteria.
Ever since the pandemic started, a lot of people ask me whether we can have bacteria kill the nasty SARS-CoV-2. I doubt it will be a direct fight between bacteria and viruses. But I am convinced that in the end bacteria and their superpowers will save this planet.
Researching and writing this post was possible due to the Journalism Research Grant from the Berlin Science Week.
it’s been a great first adventure as a proper science journalist at the #BerlinScienceWeek https://t.co/ZlJFOb9e18
— Sarah Wettstadt (@DrBommel) November 6, 2020







6 Responses
Hi Sarah,
I love this post! Very captivating and true to scientific communication.
Thank you so much for your kind words! I’m really glad you like it :)
Nice article and I appreciate you linking to our review article on vaccine design, thank you! Having a paper getting a mention in a blog is a first for me :)
Thanks for your kind words and congratulations on the great review :)
Nice job, as always Sarah and Noémi! Congrats on the grant, Sarah!! Always great to hear that good science writing is being supported and encouraged!!!!!!!
Thanks Anne!