When bacteria enter your body, the first players that act immediately belong to the so-called innate immunity. Their goal is to get rid of any intruder that may cause harm or if unable to do so, buy time for the more potent adaptive immunity to clear out an infection.
The complement system is the first line of immunity defence
As part of the innate immunity, the so-called complement system consists of several proteins. These get activated sequentially and function together to finally destroy any pathogen.
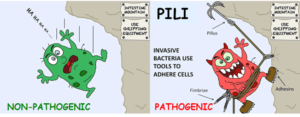
To recognise harmful bacteria, complement proteins have special receptors. These bind to specific proteins on the surface of the bacteria, so-called pathogen-associated molecular patterns, or PAMPs for short.
Imagine the bacterial PAMP as a key that perfectly fits into the groove of an immune receptor lock. The binding between these two proteins activates the immune system and triggers mechanisms that aim to clear out the pathogen.
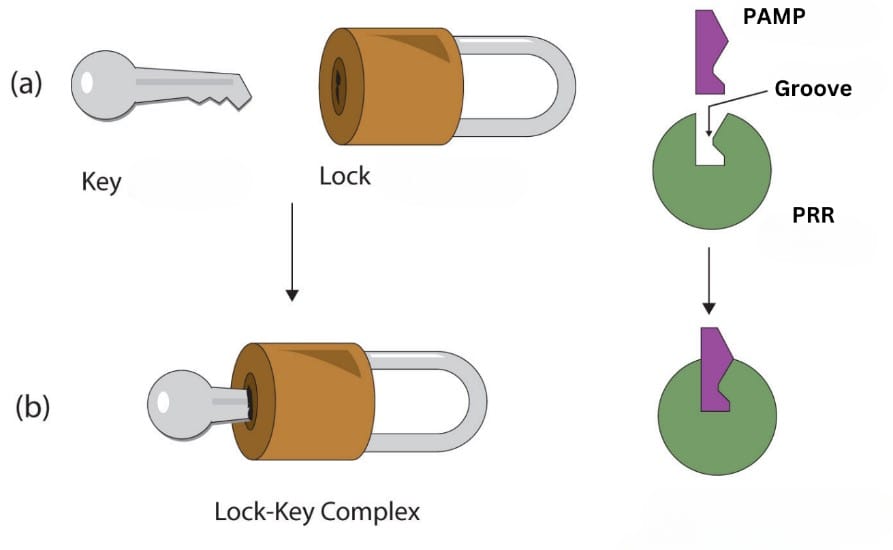
The enzymatic lock & key hypothesis.
The immune system recognising different bacteria
Bacteria come in two main types: Gram-positive and Gram-negative bacteria. Depending on which type a bacterium is, it has different PAMPs. Luckily, your immune system has evolved to identify both of these structures.
Gram-positive bacteria are surrounded by a rigid layer, the so-called peptidoglycan cell wall. Within this layer of carbohydrates and proteins are the modified carbohydrates teichoic acid and lipoteichoic acid. These are the PAMPs, that your immune system recognises and binds to.
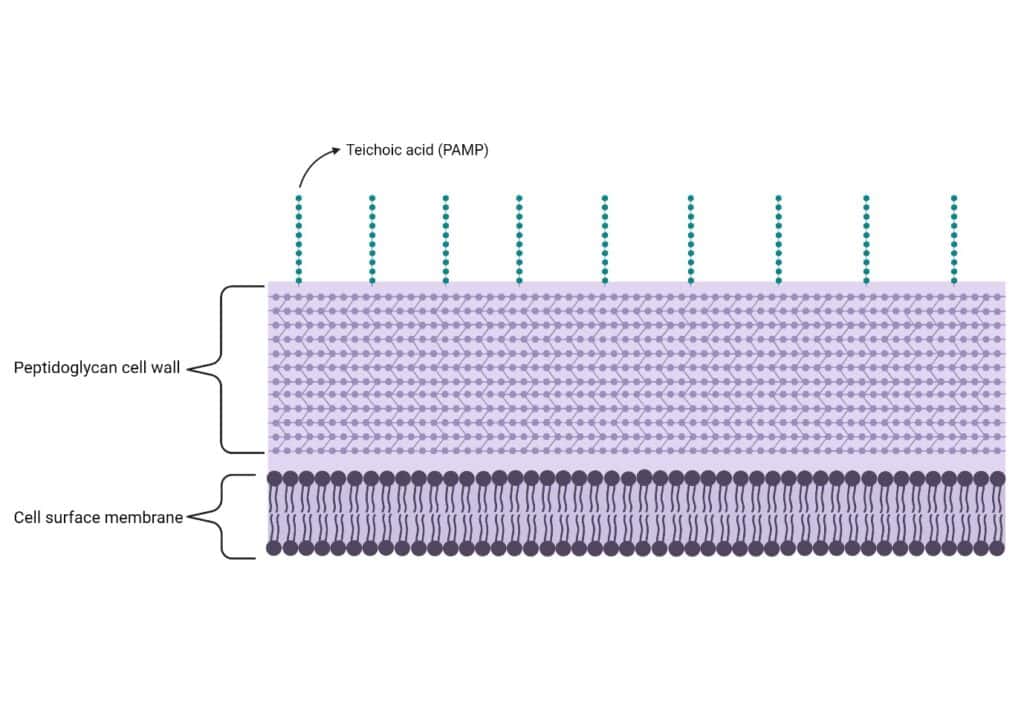
The Gram-positive bacterial cell surface. Created with BioRender.com.
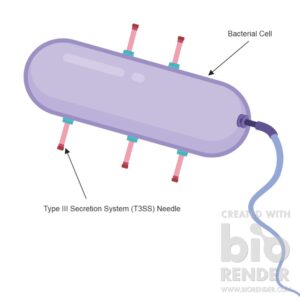
On the other hand, Gram-negative bacteria contain an additional capsule layer on top of the peptidoglycan wall. This layer is made up of another type of carbohydrate, the lipopolysaccharide, which is the PAMP of Gram-negative bacteria. So, even though Gram-negative bacteria also contain a peptidoglycan cell wall, it is covered by the capsule and thus inaccessible to the immune system.
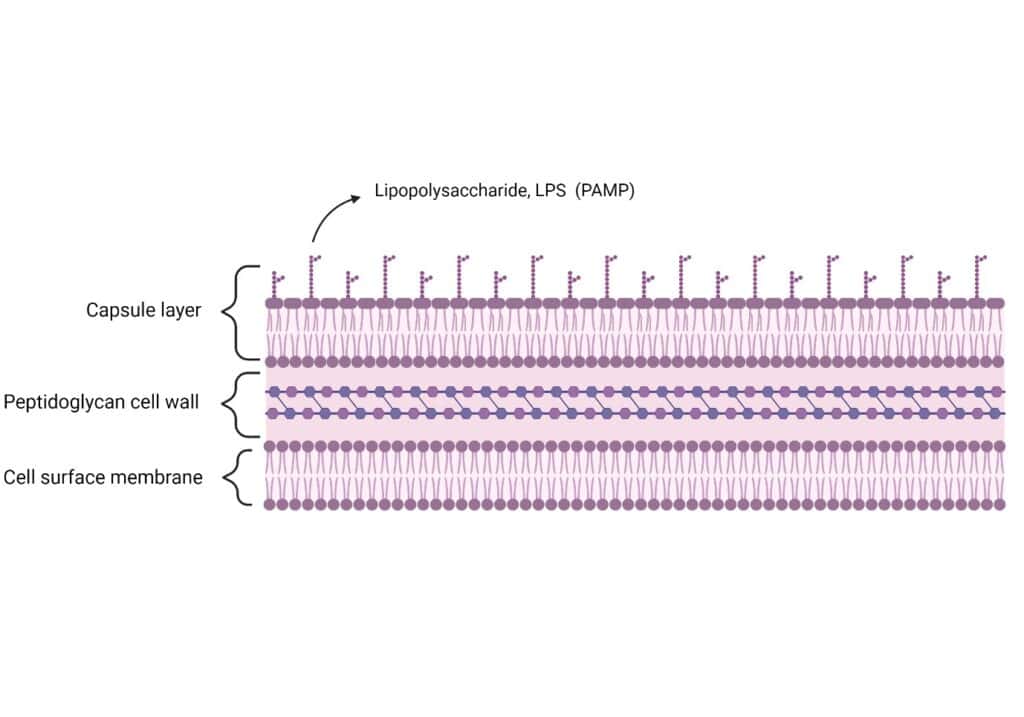
The Gram-negative bacterial cell surface. Created with BioRender.com.
How does the complement system work
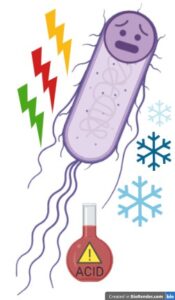
Imagine a harmful bacterium managed to sneak into your body. To prevent any intruder from causing damage, the sensor proteins of the complement system are constantly patrolling the bloodstream, hunting for malicious beings that aim to harm the body.
As soon as a sensor protein recognises and binds to a bacterial PAMP with its lock, it alerts the complement system. The sensor protein begins to produce a key enzyme called C3 convertase.
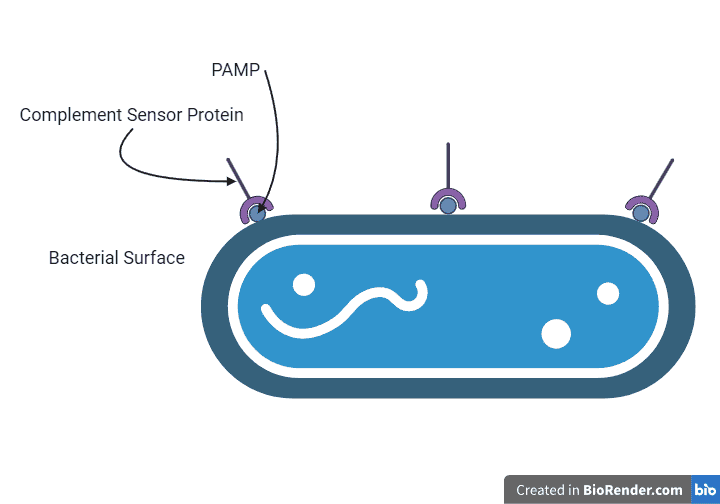
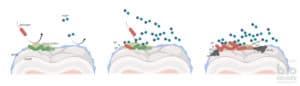
A complement sensor protein binds to a bacterial PAMP. Created with BioRender.com.
Within your blood, there are lots of small complements called C3. And the main function of the C3 convertase is to break down this C3 into small C3a and large C3b fragments. This is the most important step in complement activation and from here everything else happens.
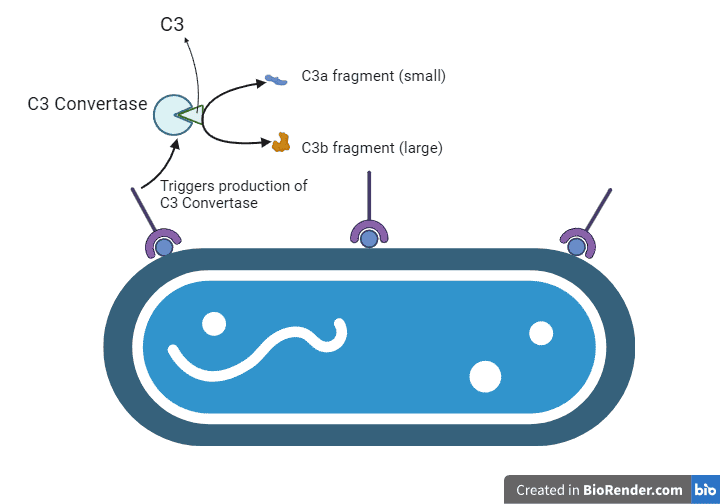
C3 convertase production and its subsequent action. Created with BioRender.com.
Now, the bloodstream is flooded with C3b fragments which bind to the bacterium’s surface. As more C3 proteins are broken down, more C3b large fragments are produced and more bind and coat the bacterium. This process is called opsonisation.
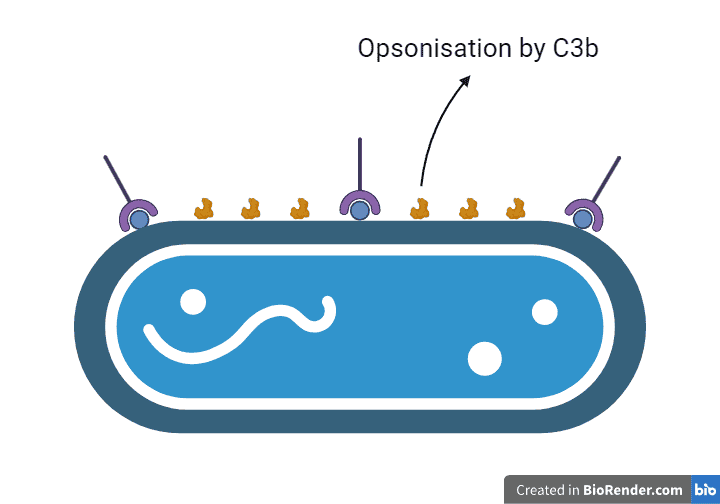
Illustration of opsonisation by C3b. Created with BioRender.com.
The immune system gets rid of bacterial intruders
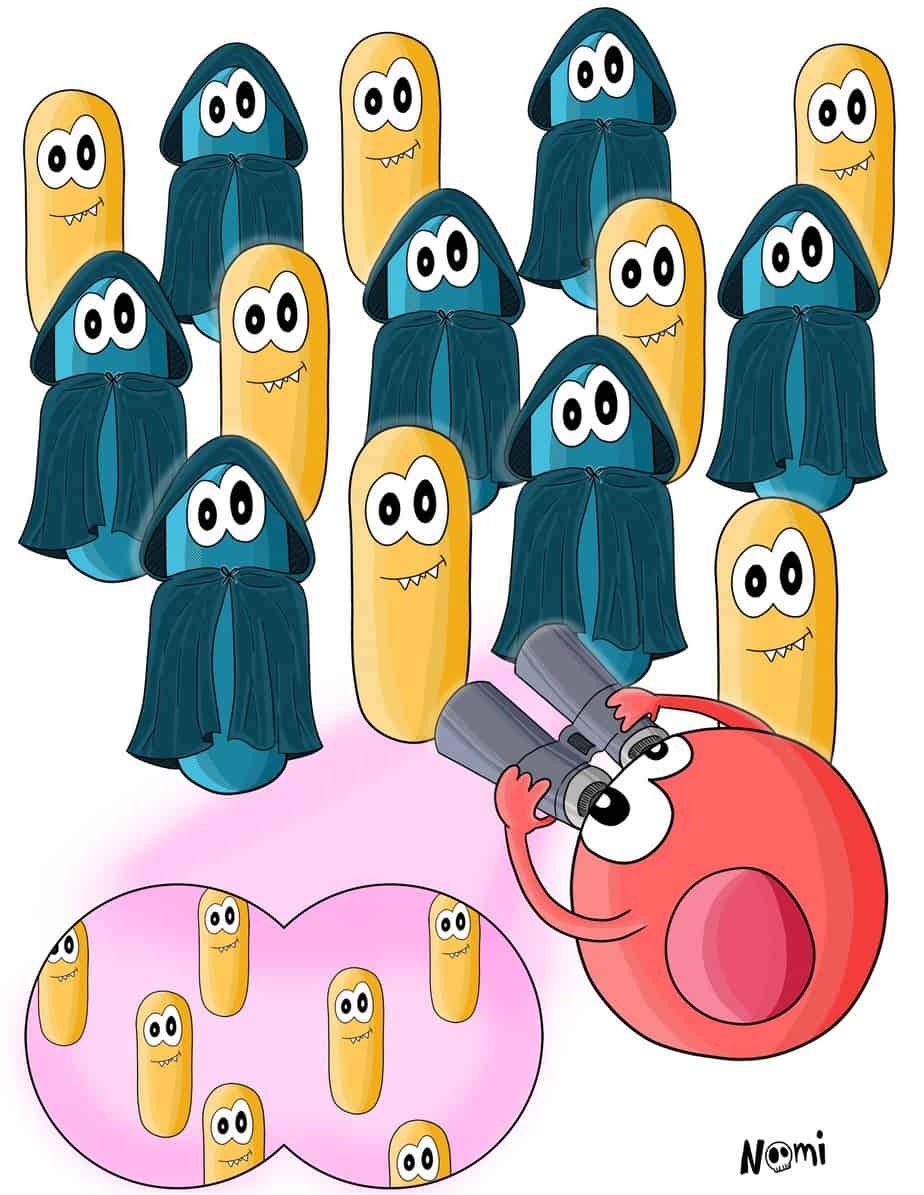
The C3b-covered bacterium now acts as a location device for phagocytes. These arrive and bind to the C3b fragment very tightly. This keeps the bacterium locked and prevents it from moving around.
Now begins the process of phagocytosis, whereby arm-like structures extend around the bacterium, eventually engulfing, ingesting and destroying it. The infection is finally cleared.
Phagocytosis of a bacterial pathogen.
In some cases, however, phagocytes do not arrive fast enough to the site where the C3b-covered bacterium hangs around. In this case, other complement proteins, such as C5 and C6, begin to spontaneously assemble around C3b and form the so-called membrane attack complex (Figure 6). This complex punctures a hole into the cell surface, which looks like a gunshot wound, causing the bacterium’s innards to spill out and dissolve.
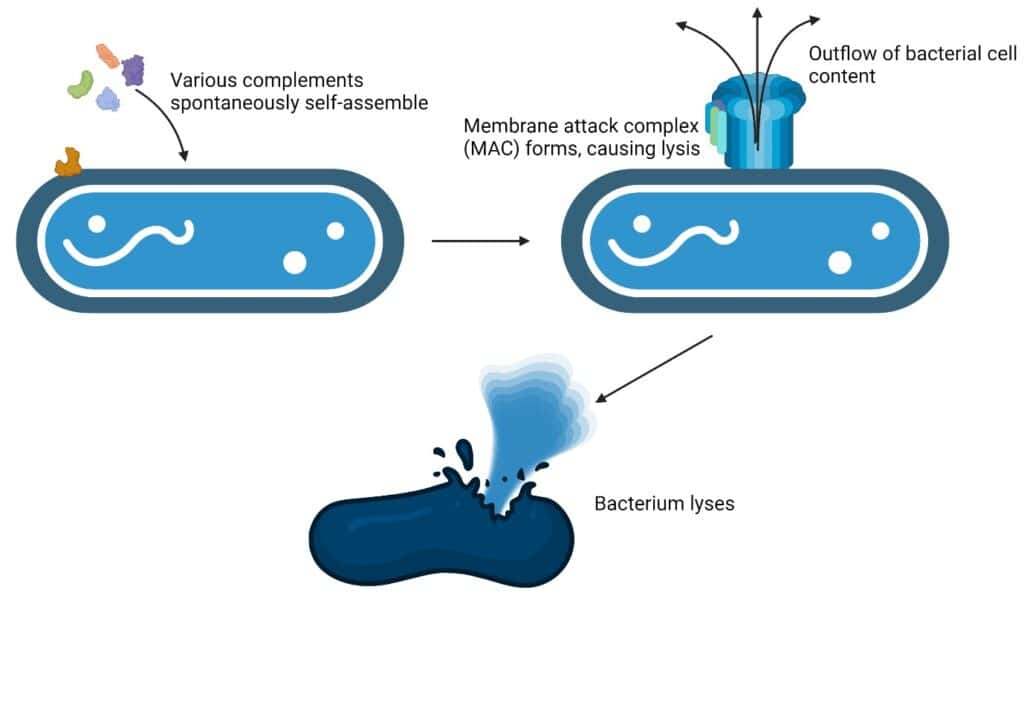
Formation of the membrane attack complex via the self-assembly of complements. Created with BioRender.com.
How does the complement system differentiate between commensal and pathogenic bacteria?
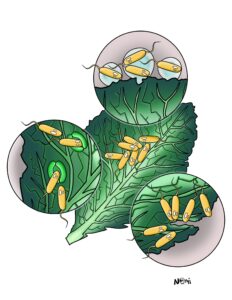
You are probably aware that in your body also live many friendly bacteria, the so-called commensal ones. And you do not want to get rid of these helpful bacteria. Hence, the immune and complement systems have adapted several strategies to keep your friendly bacteria and focus their killing power on harmful intruders.
For example, commensal bacteria reside only in certain areas of your body like the gastrointestinal tract. They do not float around in the blood. Your immune system is aware of this. Hence, the complement system in the gastrointestinal tract is modified and does not attack these commensal bacteria. Instead, their recognition skills focus on harmful intruders.
Also, commensal bacteria contain additional molecules on their surfaces to hide their PAMPs from the complement system. This prevents the complement system from getting activated.
The complement system as the first immune fighters
As you’ve seen, the complement system works tirelessly, day and night, patrolling your bloodstream to ensure that no harmful bacterium gets too comfortable inside. With its sensor proteins, it identifies these pathogens and activates the immune army to clear out any infection.
Hence, the complement system is the crucial first line of defence of our immune system. By recognizing and targeting harmful bacteria and sparing beneficial commensal bacteria, it ensures that your body remains healthy and free from infection.