When hearing the word bacteria, many people immediately think of antimicrobial resistances or short AMRs. These are a huge health issue for us since more and more resistant bugs emerge globally.
But what does it actually mean for a bacterium to be resistant to an antibiotic? What are the mechanisms behind antimicrobial resistance? And what does a resistant bacterium do once it got hit with an antibiotic?
Read on to find out the answers and learn about the basics of antimicrobial resistance mechanisms.
What does antimicrobial resistant mean?
Let’s start by looking at what an antibiotic actually is and how it works.
An antibiotic is a molecule that is supposed to stop other microbes from growing. Microbes and especially bacteria produce antibiotics to fight off other microbial foes. Some bacteria even use antibiotics to protect their hosts from other microbial intruders.
Over the years, we learned to use antibiotics as well to kill microbes like bacteria and fungi. For example, when you have a bacterial or fungal infection, you likely had to take some antibiotics. But antibiotics are useless against viruses, so we cannot use them for viral infections.
When an antibiotic hits a bacterium, the molecule binds its so-called target. This is usually an essential protein within the bacterium. And binding this target prevents it from working properly. But the functioning of the protein is essential for the bacterium, it cannot grow anymore and eventually dies.
Now, there are two options: the antibiotic has such a target within the bacterium and can stop this target from working. This kills the bacterium, which is hence called antibiotic sensitive. If however, an antibiotic does not have an effect on a bacterium, the bacterium is called antibiotic-resistant.
But where do these antimicrobial resistance mechanisms come from? How does a bacterium become resistant to a drug?
Where do antimicrobial resistance mechanisms come from?
Antimicrobial resistance mechanisms have two major sources.
An intrinsic resistance means that a bacterium is naturally resistant to a specific antibiotic. It has these antimicrobial resistance mechanisms from the day it was born.
For example, some antibiotics target specific components within a bacterial cell. This could be the production machinery of the membrane of the bacterium. But then, we know that the membranes of Gram-positive bacteria and Gram-negative bacteria are different. And some antibiotics only work against one of them. So, some bacteria are resistant to certain antibiotics because they have different machineries that produce the membranes.
On the other hand, there are acquired resistances. This is when a bacterium gained or acquired that resistance during its lifetime. This usually happens when bacteria mutate.
Another possibility is that a bacterium takes up DNA from another resistant bacterium. Then the bacterium also gains the superpower to fight off the antibiotic.
But what actually happens with the antibiotic in a resistant bacterium?
What are antimicrobial resistance mechanisms?
As we said, antibiotics can look and work differently. Hence, bacteria worked out different mechanisms to get rid of the harmful molecule. Here, we will look at the best-understood examples of antimicrobial resistance mechanisms.
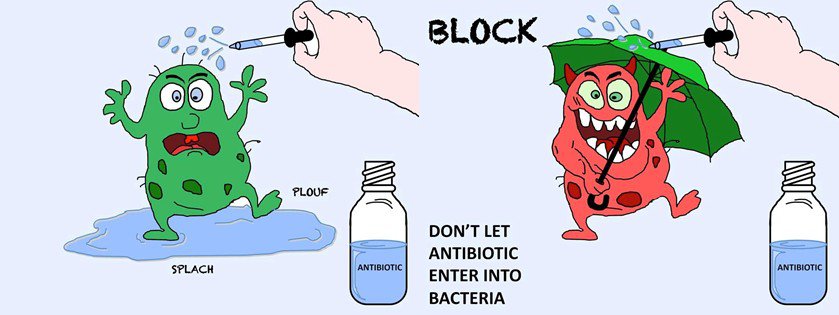
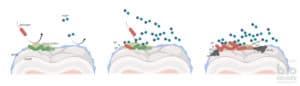
Blocking the antibiotic from entering
All bacteria produce transporters that import stuff from the outside into the cell. Some of these transporters also import antibiotics. And often a bacterium realises that antibiotics enter the cell via a specific transporter. In this case, the bacterium decides to produce less of this transporter.
Another possibility is that the bacterium changes the transporter. It might still transport its normal substrate but not the antibiotic anymore. With this, the bacterium makes sure that the antibiotic never actually enters the cell.
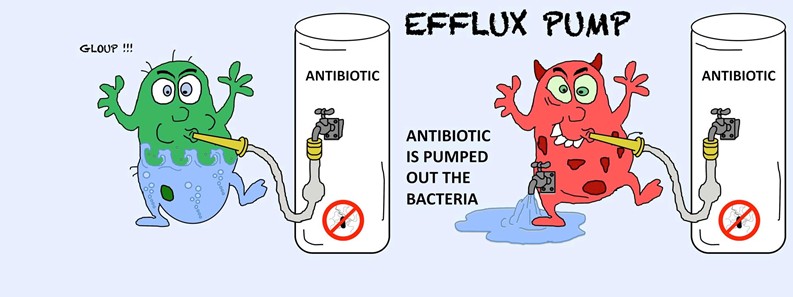
Getting rid of the antibiotic
As soon as an antibiotic entered the cell, bacteria can also get rid of it.
For this, bacteria produce efflux pumps. These generally export all sorts of cellular waste and some of these can also export antibiotics. When a bacterium realises that there are antibiotics inside the cell, it produces a lot of these efflux pumps. With this, the bacterium gets rid of the incoming antibiotics quickly.
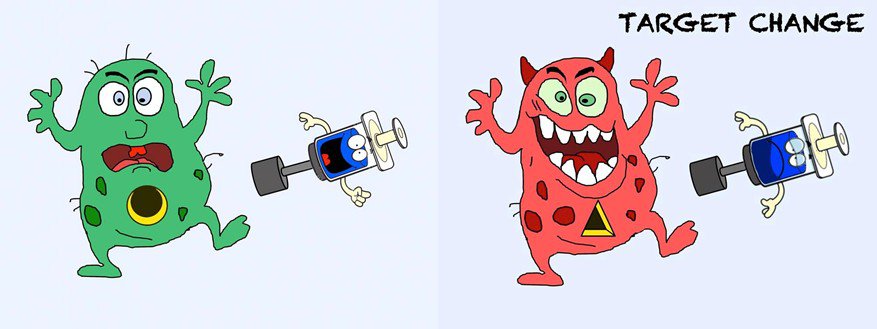
Changing the antibiotic target
Within the bacterium, the antibiotic binds to its specific target and prevents it from working. However, bacteria can change or mutate this target so that the molecule cannot bind to it anymore. This makes the antibiotic useless.
Yet, the function of the target is usually essential for the bacterium’s survival. So, when changing the target, the bacterium needs to make sure to only prevent antibiotic binding and that the target itself still works.
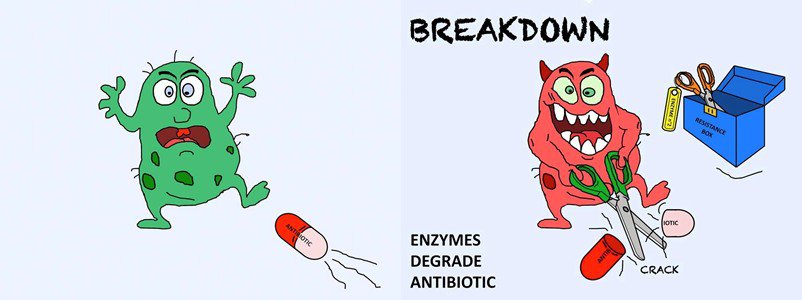
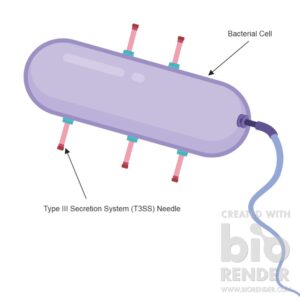
Inactivating the antibiotic
Bacteria also found ways to get rid of the molecule by breaking them apart. For this, they produce proteins that completely break the antibiotic or change it slightly. This stops the antibiotic from binding to its target and the antibiotic is useless.
Unfortunately, bacteria have many different proteins to break or change antibiotics. And researchers keep finding more and more of them making it harder for us to fight off resistant bugs.
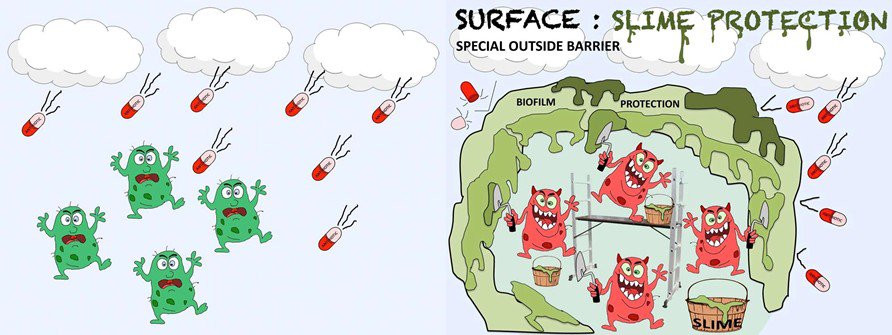
Covering in biofilm
Some bacteria have the ability to build a so-called biofilm, which is basically a lot of slime in which bacteria can live and grow.
This slime is like a house that protects from danger. So, no antibiotic can enter and all bacteria inside this slime house are protected. Building such a biofilm house is more of a general protection strategy. It just happens that it is also very efficient against antibiotic attacks.
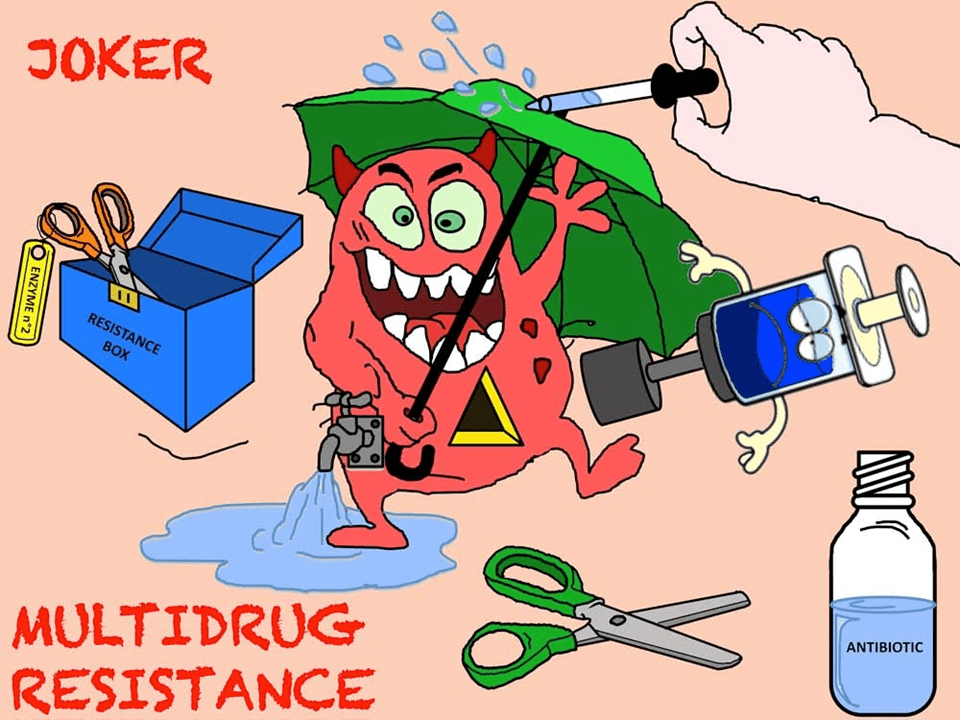
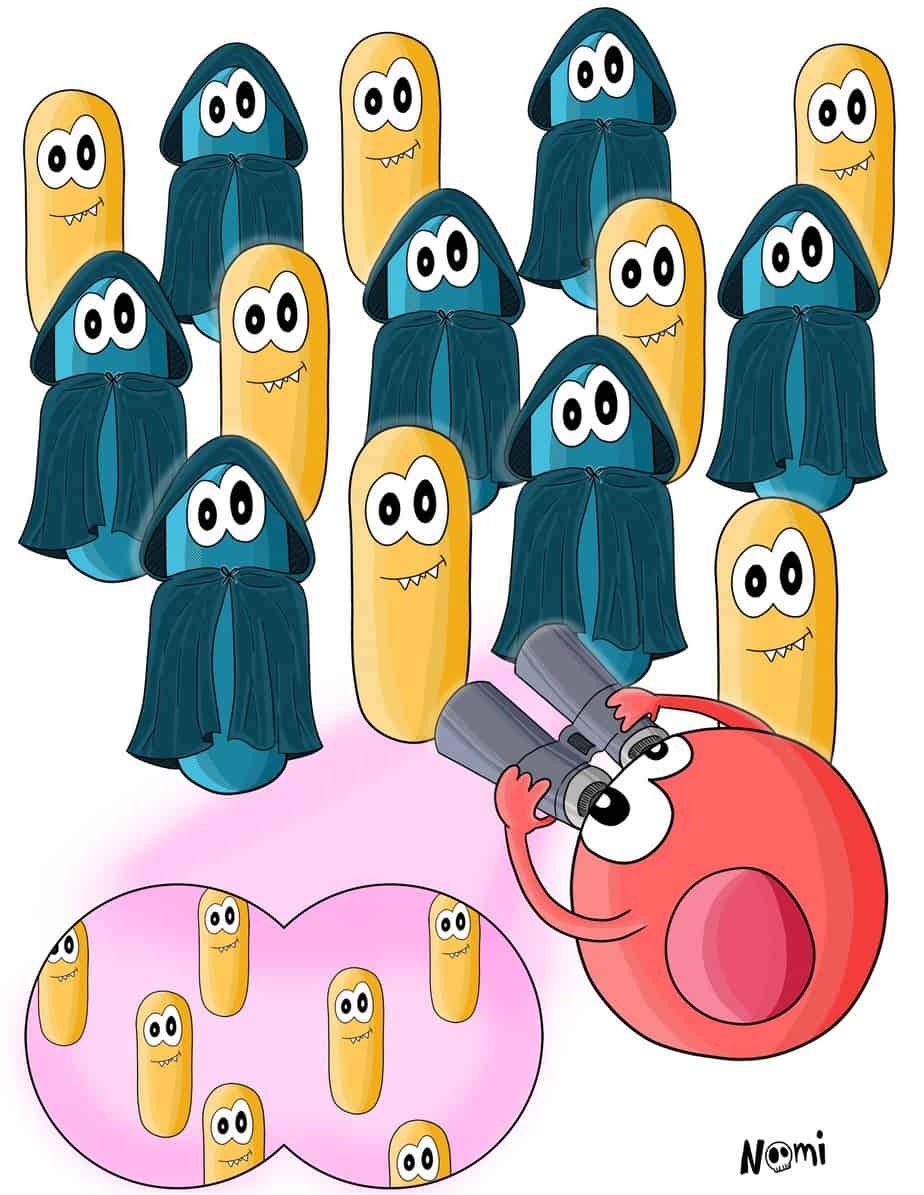
The Joker – having many antimicrobial resistance mechanisms
Now you know that there are different resistance mechanisms to fight off antibiotics. But, imagine a bacterium does not only have one of these mechanisms but several of them.
In this case, the bacterium knows how to get rid of many different antibiotics. So, even though we have a lot of antibiotics available, none of them work. And this is what they call a multi-drug resistant bacterium – or superbug – as these are resistant to many different antibiotics.
Antimicrobial resistance mechanisms are serious
And researchers keep finding new ways of how bacteria get rid of antibiotics. For example, a new study found that bacteriophages can protect bacteria from antibiotics in a completely new mechanism.
This is a serious problem as you can imagine. If we do not have any more drugs to fight bacteria, they will just keep making us sick. This will eventually lead to more and more deaths caused by bacterial infections.
And this is why research is so important. One major challenge for scientists right now is to find alternative anti-microbial drugs to which bacteria cannot become or hardly become resistant.


9 Responses
Mit grosser Interesse den Artikel gelesen und sehr anschaulich und verständlich.Danke
Dank dir
Hi there,
Love this blog. For someone new to AMR and trying to write an AMR surveillance plan for our jurisdiction this is helpful. I feel like I’m starting to understand the different mechanisms now.
I understand that another mechanism is the role of plasmids? – could this be an idea for a similar blog.
Thanks,
Callum
(Australia)
Hi Callum, thanks a lot for your feedback. I am very glad it is useful for you.
Yes, in plasmids the genes for different AMRs are encoded and by spreading the plasmids the AMRs are spread. An article about horizontal gene transfer as a means to spread plasmids will likely be coming soon. So keep an eye on this place ;)
Good day! I could have sworn I’ve visited your blog before but
after looking at many of the articles I realized it’s new to me.
Regardless, I’m definitely happy I stumbled upon it and I’ll be
book-marking it and checking back frequently!
Thank you! Enjoy reading it!
I hope asap the world ll come up with sturdy antibiotic drugs